Defending T3 levels is a priority yet the majority still do not test it
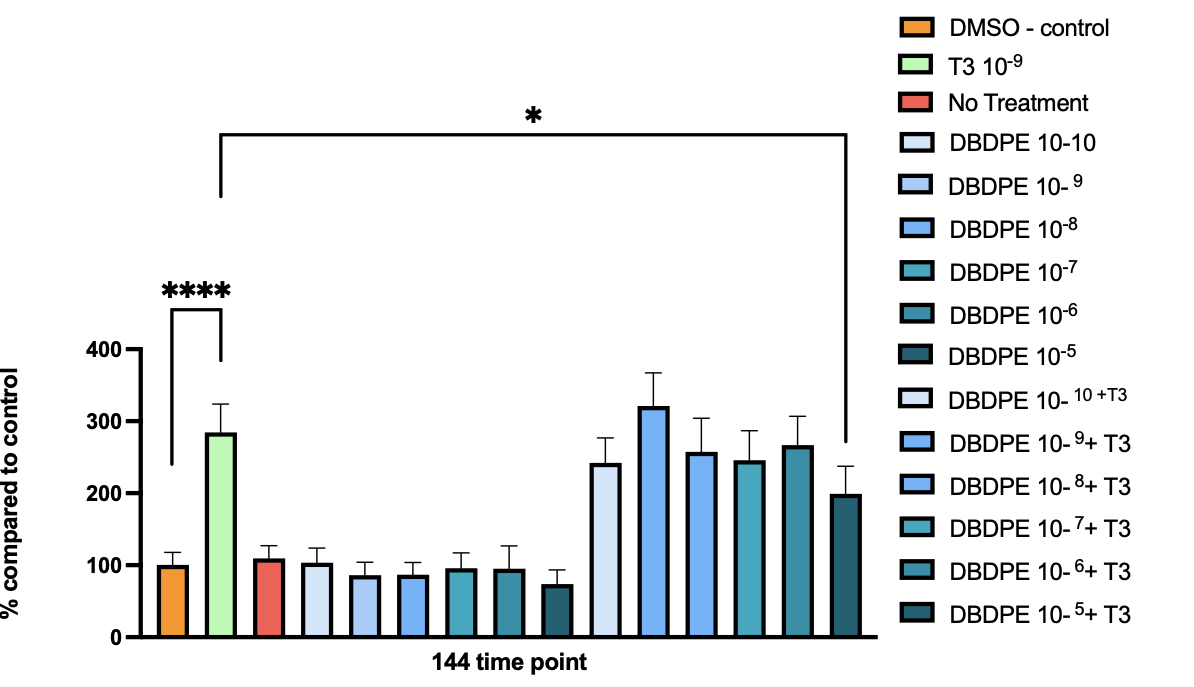
I thought it was time to add some quick reads or it will be another three years of research and little said about why or what I am doing with this research. I’ve written previously about the necessity of T3 and my current research in a rat pituitary (GH3) cell line is reduced yet useful for defending T3 values.
T3 is a proliferative hormone that also promotes differentiation. In this GH3 cell line, despite exposure to a flame retardant, the effects of T3 are largely not affected until the dose gets high. This could be a problem with chronic bioaccumulation of these and other lipophilic (fat loving) compounds.
T4 is often considered a “pre hormone” as it converts to T3 but in reality it can bind to nuclear receptors in limited fashion but more importantly has high affinity with the integrin avß3 which can promote proliferation and angiogenesis. T4 is still the drug of choice for restoring euthyroidism based upon the unstable foundation that both TSH below 4.5 mu/L and adequate T4 in the reference range predicts thyroid health.
Observations in those prescribed thyroxine chronically suggest a 50% increased risk of brain, skin, pancreatic and breast cancers (AOR: 1.50, 95% CI 1.46 – 1.54; P<0.0001) compared with non-users, albeit the link is only associational (Wu et al., 2021).
Environmental factors could exacerbate these proliferative and angiogenic effects of T4 that could bind to the integrin receptor as thyroid mimicks and increase T4 like responses. Unfortunately, despite the well documented features of the hypothalamic pituitary feedback loop, adequate T3 may not be able to get into the cell, where the majority of systemic T3 stores should be. The state at large could drive a low thyroid proinflammatory pathway where TSH is not reduced. Increased TSH within the normal range is associated with poor insulin and glucose regulation metabolic syndrome and PCOS and is part of the pro-inflammatory state (Mueller et al., 2009; Ruhla et al., 2010).
TSH and FT4 merely represent circulating values of these hormones, they are effectively a marker of output based upon production and uptake. If any aspect of thyroid transport or uptake is perturbed, the values assessed in the serum are not reflective of chemical binding to serum transporters, and potential effects on transmembrane transporters, deiodination, binding of non-ligand to receptors and reduced hypothalamic sensitivity to circulating TH.
Interestingly, some researchers suggest a mathematical modelling approach and consideration of evaluation of FT3 as a more nuanced approach to predicting thyroid disease when the hypothalamic pituitary axis has been perturbed (Hoermann, Pekker, Midgley, & Dietrich, 2023). They stress that FT3 output is only as productive as the system that is in operation. In a world where we are bombarded with endocrine insults, electromagnetic, emotional and dietary stressors it doesn’t need too much thought to understand why such an axis could be perturbed. Even that amazing mRNA technology that would prevent transmission of a novel disease, and prevent severity appears to increase hypothyroidism (Sungho Bea, Hwa Young Ahn, Jieun Woo, Ju-Young Shin, n.d.).
In most of my research to date I have found that T3 rescues the effects of reduced thyroid induced proliferation and decreases cytotoxicity of cells by reducing lactate dehydrogenase and glycolytic metabolism of failing cells. Although in extreme exposures of thyroid disrupters or where bioaccumulation occurs this may not be the case. However adequate T3 would ensure that bioaccumulation is less likely. Also, adequate retinol ensures that compounds like bisphenol A are detoxified through up regulation of the thyroid stabilising retinoid X receptor (RXR) which functions in tandem (heterodimerizes) with not just the thyroid receptors but the pregnane X receptors (PXR) and constitutive androgen receptors (CAR) which promote metabolism through hepatic/liver CYP enzyme pathways.
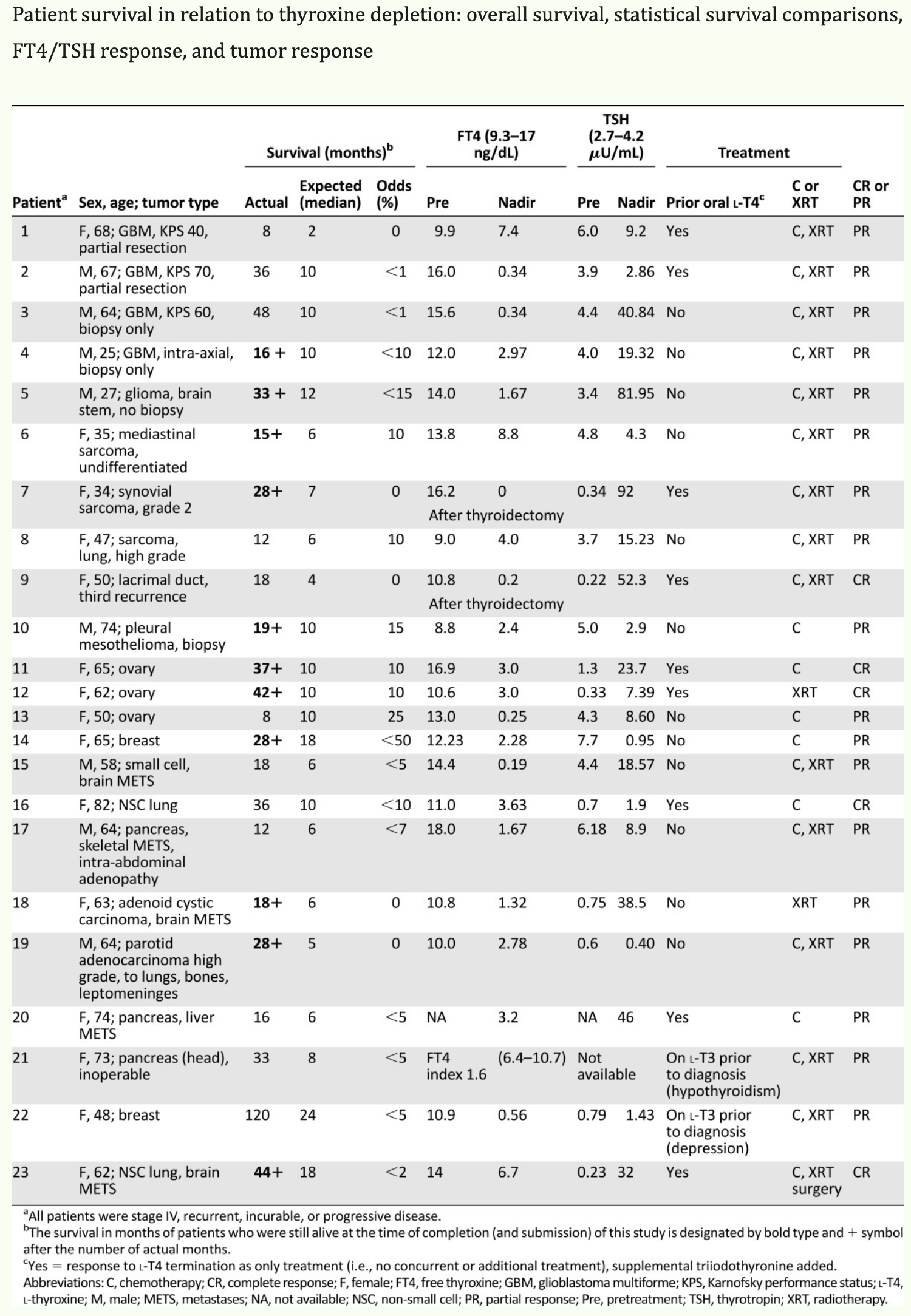
I found the paper below interesting, as it supports the notion that lowering the proliferative effects of T4 and maintaing T3 status with triiodothyronine supplementation increases lifespan. Either that or the clinician’s were really bad at predicting mortality. It’s associational, so not a lot of weight can be placed on the effects. Chemotherapy and radiation are heavy insults that are thyroid suppressive ensuring availability of T3 has more logic than the standard care of Levothyroxine.
References:
Escobar-Morreale, H. F. F., Botella-Carretero, J. I., & De Escobar, G. M. (2015). Treatment of hypothyroidism with levothyroxine or a combination of levothyroxine plus L-triiodothyronine. Best Practice and Research: Clinical Endocrinology and Metabolism. https://doi.org/10.1016/j.beem.2014.10.004
Hoermann, R., Pekker, M. J., Midgley, J. E. M., & Dietrich, J. W. (2023). The role of supporting and disruptive mechanisms of FT3 homeostasis in regulating the hypothalamic–pituitary–thyroid axis. Therapeutic Advances in Endocrinology and Metabolism, 14. https://doi.org/10.1177/20420188231158163
Mueller, A., Schöfl, C., Dittrich, R., Cupisti, S., Oppelt, P. G., Schild, R. L., … Häberle, L. (2009). Thyroid-stimulating hormone is associated with insulin resistance independently of body mass index and age in women with polycystic ovary syndrome. Human Reproduction. https://doi.org/10.1093/humrep/dep285
Ruhla, S., Weickert, M. O., Arafat, A. M., Osterhoff, M., Isken, F., Spranger, J., … Möhlig, M. (2010). A high normal TSH is associated with the metabolic syndrome. Clinical Endocrinology, 72(5), 696–701. https://doi.org/10.1111/j.1365-2265.2009.03698.x
Shmarakov, I. O., Borschovetska, V. L., & Blaner, W. S. (2017). Hepatic detoxification of Bisphenol A is retinoid-dependent. Toxicological Sciences, 157(1). https://doi.org/10.1093/toxsci/kfx022
Sungho Bea, Hwa Young Ahn, Jieun Woo, Ju-Young Shin, S. W. C. (n.d.). Effect of COVID-19 Vaccination on Thyroid Disease in 7 Million Adult and 0.2 Million Adolescent Vaccine Recipients. The Journal of Clinical Endocrinology & Metabolism, Volume 110.
De